Utilization of Tibio-Pedal Artery Minimally Invasive Approach to Treat Complex Below Knee Disease in a High Transfemoral Risk Patient
Zola N’Dandu, MD, and Jonathan Bonilla, MD
John Ochsner Heart and Vascular Institute, Ochsner Medical Center-Kenner, Kenner, Louisiana
With the evolution of endovascular techniques, historically untreated patients have options. Tibio-pedal artery minimally invasive (TAMI) approach is safe and feasible when avoiding transfemoral access complications. 1-3
Case Report

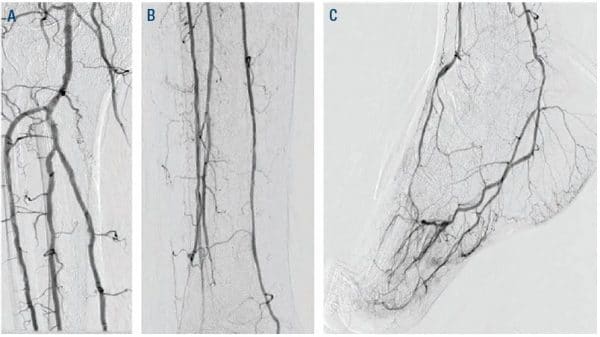
Figure 1. Diagnostic angiogram: ATA CTO, patent PTA, patent PER, and patent LPA. ATA = anterior tibial artery; CTO = chronic total occlusion; PTA = posterior tibial artery; PER = peroneal; LPA = lateral plantar artery.
A 66-year-old male with a past medical history of hypertension, hyperlipidemia, insulin-dependent diabetes mellitus Type 2 for more than 20 years, coronary artery disease previously treated with multivessel percutaneous coronary intervention (PCI), ischemic cardiomyopathy with ejection fraction of 35%, morbid obesity with body mass index (BMI) of 52, and sleep apnea presenting with chronic limb threatening ischemia (CLTI), presented with necrotizing fasciitis requiring an urgent debridement for infection control. His non-invasive vascular workup included an abnormal ankle brachial index (ABI), an abnormal arterial ultrasound, and tissue oximetry.
He had a right transradial aortogram with selective right leg angiogram. His angiogram revealed adequate inflow with patent aorto-iliac, common femoral, superficial femoral, profunda, and popliteal vessels. Distally he had a chronically occluded (CTO) right anterior tibial (ATA) with a hibernating dorsalis pedis artery (DPA), which faintly filled from a peroneal (PER) collateral, 90% tibial peroneal trunk (TPT) stenosis, multiple 75% lesions in the proximal and mid posterior tibial artery (PTA), and a patent lateral plantar artery (LPA) (Figure 1).

Figure 2. Retrograde 2.9 Fr ATA and 4-5 Fr PTA sheaths. ATA = anterior tibial artery; PTA = posterior tibial artery.
Anticipating a high risk of complications related to transfemoral access, we decided to proceed with TAMI approach with transradial guidance. A 4- to 5-Fr Glidesheath Slender (GSS) (Terumo Medical) was inserted in the right radial artery for visualization of the proximal vessels. We placed a 2.9-Fr Cook pedal (Cook Medical) sheath in the ATA and advanced a 0.018-inch CXI (Cook Medical) support catheter over a 0.018-inch Command ST (Abbott Vascular) wire. The CXI catheter and wire were advanced through the course of the ATA intraluminally except for the ostium of the ATA where the wire entered a subintimal space. Thereafter, we gained access in the right PT with a 4- to 5-Fr GSS sheath to serve as an antegrade access to cross the ATA CTO (Figure 2). A 0.018-inch CXI support catheter was telescoped within a 4-Fr Berenstein (Boston Scientific) catheter with a 0.018-inch Command wire advanced into the proximal ATA (Figure 3). The antegrade equipment was advanced into the distal ATA. The retrograde CXI catheter was pulled back in the distal AT where the antegrade wire was inserted for externalization. Subsequently the antegrade CXI catheter was externalized through the retrograde 2.9-Fr sheath placed in the distal ATA (Figure 4). The 0.018-inch Command wire was exchanged for a 0.014-inch ViperWire (Cardiovascular Systems, Inc.) guidewire to perform therectomy using a 1.5 mm Classic CSI Diamondback 360 catheter in the PTA, TPT, and ATA (Figure 5). Thereafter, based on extra vascular ultrasound (EVUS) measurements, we performed balloon angioplasty of proximal DPA, ATA, and PTA with a 3.5-x 300-mm balloon (Ultraverse BD Bard), and TPT with a 4.0- x 60-mm Lutonix DCB (BD Bard) with an excellent result (Figure 6).
To reduce the risk of access-related complications, we usually perform balloon tamponade with 2.5- or 3.0-mm Advance Micro 14 2.5-Fr balloon through a distal 2.9-Fr sheath which can safely be closed with minimal manual pressure.
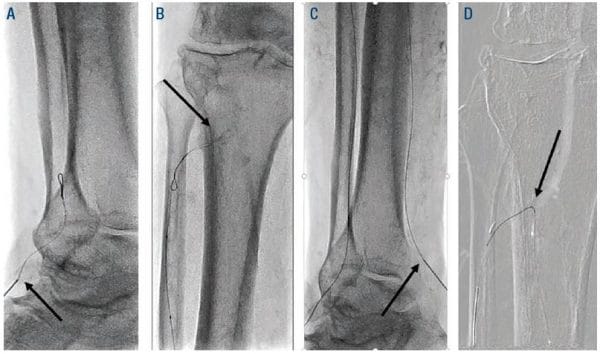
Figure 3. Arrow (A) retrograde ATA access, (B) retrograde wire looped at ATA ostium, (C) retrograde PT access, (D) retrograde PTA crossed into proximal ATA. PT = posterior tibial; PTA = posterior tibial artery; ATA = anterior tibial artery.
A 3.0- x 80-mm Advance Micro 14 2.5-Fr (Cook Medical) balloon was inserted through the retrograde ATA 2.9-Fr sheath over the ViperWire guidewire which was exchanged for a 0.014-inch Fielder XT (Asahi Intecc) and advanced distally to the 4- to 5-Fr GSS PTA access for intraarterial balloon tamponade to obtain hemostasis (Figure 7). Finally, the retrograde 2.9 Fr ATA sheath was removed, and hemostasis was achieved with manual pressure (Figure 8). He tolerated the procedure well and ambulated an hour later. He underwent additional debridement and placement of a wound vac.
The TAMI approach has been well documented. It can be utilized as an alternative in patients with high risk of complications related to transfemoral access. In other cases, we used up to 5 to 6 and 6 to 7 GSS sheaths. To reduce the risk of access-related complications, we usually perform balloon tamponade with 2.5- or 3.0-mm Advance Micro 14 2.5-Fr (Cook) balloon through a distal 2.9-Fr sheath which can safely be closed with minimal manual pressure (Figure 9). We always utilize a hockey stick ultrasound probe to obtain access. We maintain an ACT greater than 250 seconds during the
case. We inject between 200 or 400 mcg of intra-arterial nitroglycerin for vasodilation and repeat the same process every thirty minutes.

Figure 4. Oval (A) antegrade and retrograde wires in ATA and arrow (B) externalization of antegrade wire through the retrograde ATA access. ATA = anterior tibial artery.
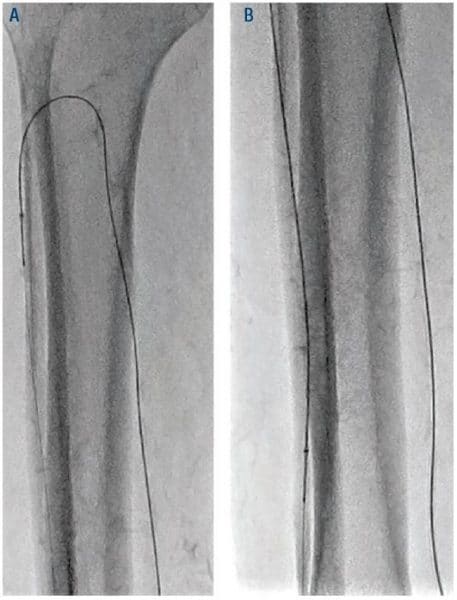
Figure 5. Atherectomy of ATA through PTA access with 1.5 Classic CSI catheter. ATA = anterior tibial artery; PTA = posterior tibial artery; CSI = Cardiovascular Systems, Inc.
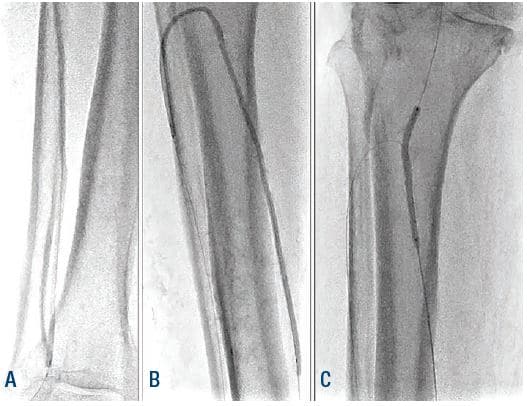
Figure 6. Angioplasty of ATA, PTA, and TPT. ATA = anterior tibial artery; PTA = posterior tibial artery; TPT = tibial peroneal trunk.
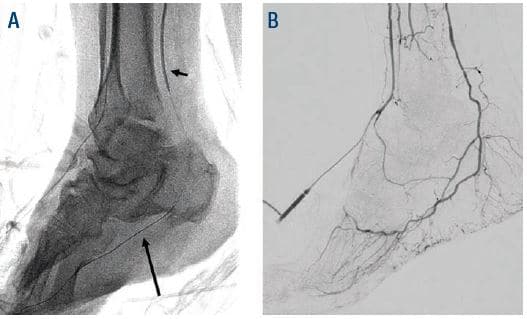
Figure 7. (A) Short arrow points to PTA access balloon tamponade, long arrow is pointing at Fielder XT. (B) Successful hemostasis.

Figure 9. TAMI with a 5-6 Fr GSS and a distal 2.9 Fr sheath inserted at the end of the case for balloon tamponade of the 5-6 Fr sheath with 3.0 mm Advance Micro (Cook) balloon. GSS = Glidesheath Slender (Terumo Medical).
Reprinted from Vascular Disease Management 2020; May, Vol. 17(5): E92-E94.
References
- Mustapha JA, Saab F, McGoff TN, et al. Tibiopedal arterial minimally invasive retrograde revascularization (TAMI) in patients with peripheral arterial disease and critical limb ischemia. On behalf of the Peripheral Registry of Endovascular Clinical Outcomes (PRIME). Catheter Cardiovasc Interv. 2020;95(3):447-454. Epub 2019 Dec 13.
- Mustapha JA, Saab F, McGoff T, et al. Tibio-pedal arterial minimally invasive retrograde revascularization in patients with advanced peripheral vascular disease: the TAMI technique, original case series. Catheter Cardiovasc Interv. 2014;83:987-994.
- Welling RHA, Bakker OJ, Scheinert D, et al. Below-the-knee retrograde access for peripheral interventions:a systematic review. J Endovasc Ther 2018;25:345–352.